Prochant seamlessly integrates advanced technology with our expert staff to provide comprehensive revenue cycle management solutions that optimize operations, enhance financial performance and elevate patient satisfaction across the home-based care industry. We leverage AI and automation across the entire revenue cycle to enhance accuracy and efficiency, from automating routine tasks and predicting denials to optimizing billing processes and streamlining claims management.
Elevating Revenue Cycle Management
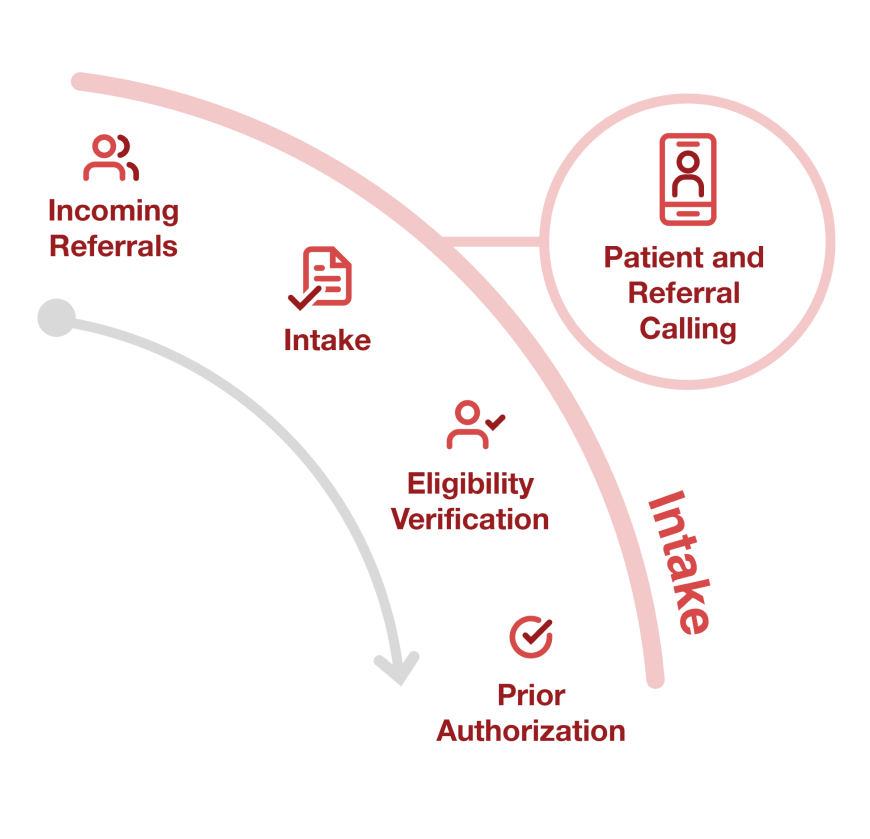
Prochant’s Engagement Services streamline patient and referral communications, helping providers optimize their revenue cycle. Our team manages patient follow-ups, insurance updates, referral acknowledgments and more, using tailored scripts and advanced tracking tools. With a best practices approach built upon cost-effective staffing and high-quality interactions and industry-leading performance metrics, we ensure quality and patient satisfaction while reducing the administrative burden on your team.
Benefit: By expertly managing incoming referrals and securing prior authorizations, Prochant reduces costly denials, leading to improved financial outcomes and more efficient revenue cycles.
Benefit: Through comprehensive oversight of demographic data entry, eligibility verification and prior authorization processes, Prochant reduces administrative complexities, streamlining the intake process for better overall efficiency.
First Call Resolution
Customer Satisfaction Score
Quality Assurance Score
Optimizing referrals, reducing denials
Our Intake Service, powered by advanced technology, efficiently directs incoming referrals and secures prior authorizations, strategically reducing backend issues such as denials. This ensures a smoother workflow, reduces administrative complexities, and enhances overall operational efficiency. By leveraging intelligent algorithms and AI, we are able to track workforce productivity and quality and streamline eligibility verification and prior authorization (EVPA) within Prochant’s Intake service. This real-time visibility allows us to ensure that processes are handled accurately and efficiently, minimizing errors and delays.
- Document Wrangling: Import new documents into the system and direct the images to the appropriate workgroup and queue.
- Incoming referrals: Review and retrieval of incoming referrals, routing of referrals to correct team for further intake processing.
- Intake: Demographic data entry, order entry, indexing and filing of electronic medical records.
- Eligibility Verification: Verification of benefits, coverage, insurance data entry and documentation of verification notes.
- Prior Authorization: Request of initial prior authorizations via web portal, fax and associated follow up.
Automating billing, improving cash flow
Our Billing Service handles the entire billing process, from generating invoices and submitting claims to managing payer rejections, ensuring accuracy, reducing administrative burdens and improving cash flow efficiency. Through automation and intelligent software, we have automated claim submissions, streamlined error detection and enhanced billing accuracy.
- Hold Management: Review of all claims on hold, identify steps to cure holds, attempt to release or route for follow up via logging CMN’s, Orders, PAR’s or other medical documentation.
- Billing Review: Pre-review of all claims ahead of transmission to identify missing or invalid claim elements.
- Claims Transmissions: Batching of claims and submission to payer or clearinghouse. Direct entry to clearinghouse and paper claims.
- Front End Rejections: Identify, research and resolve claims rejected by the clearinghouse/payer.
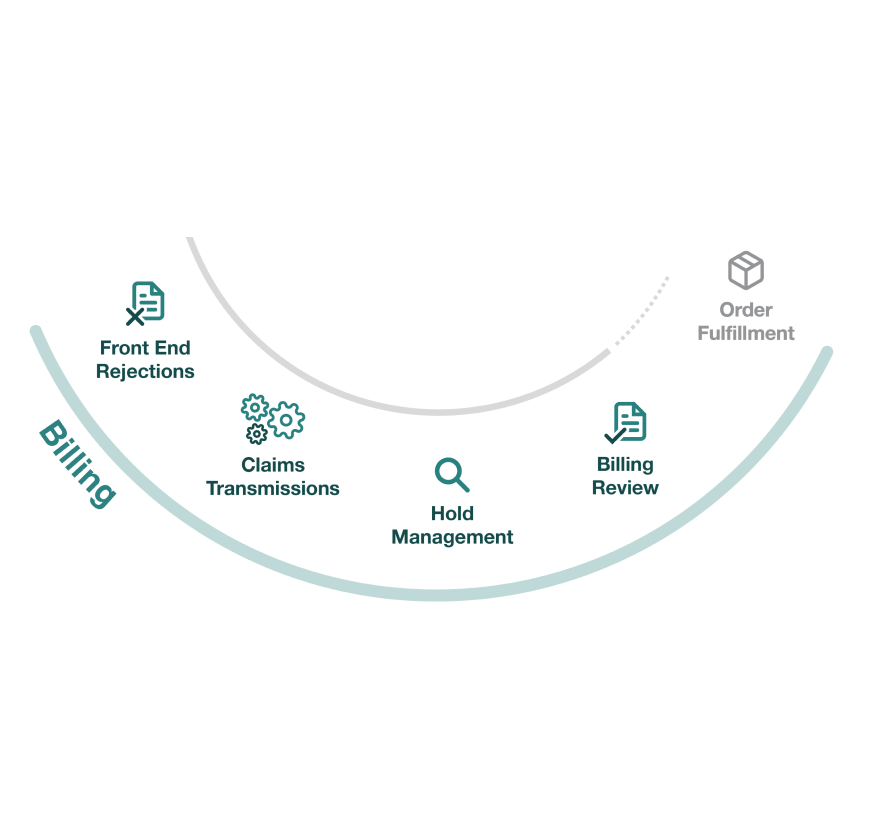
Benefit: Our billing service ensures accurate invoice generation, claim submission and prompt resolution of rejections, leading to improved cash flow efficiency and more reliable financial outcomes.
Benefit: By managing the entire billing process, we significantly reduce the administrative workload, allowing your team to focus on higher-priority task.
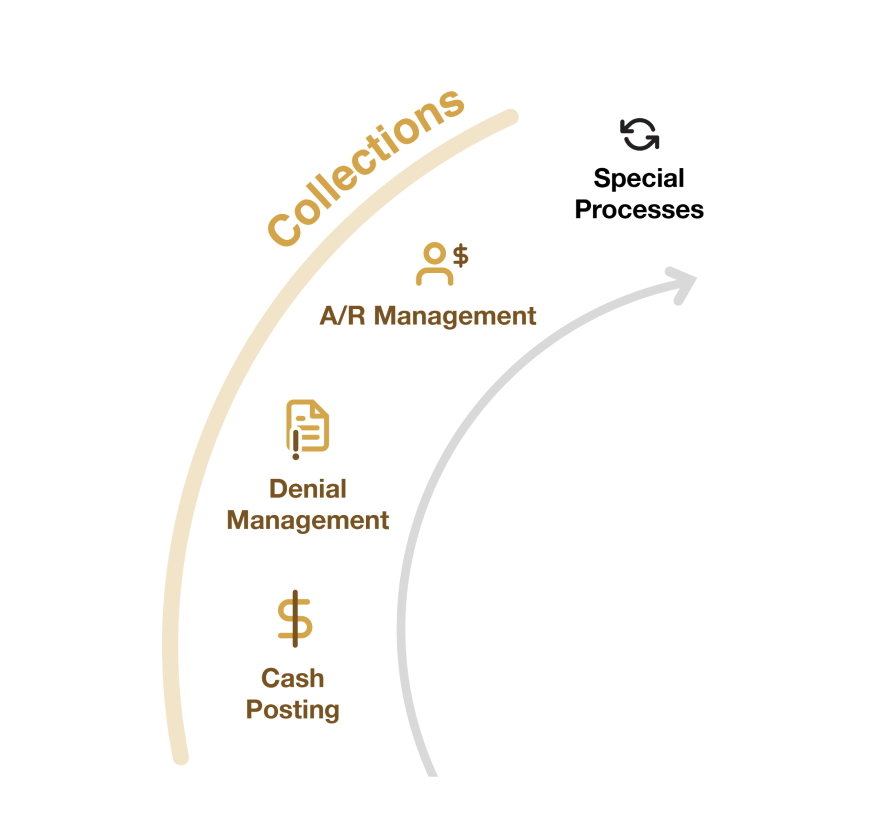
Benefit: Our comprehensive management of recovery and cash posting speeds up payments and maximizes the recovery of outstanding bills.
Benefit: By efficiently handling cash posting, denial management and AR follow-ups, we minimize the time and effort required to recoup unpaid invoices, streamlining the collections process.
Accelerating payments, maximizing recovery
Our Collections Service manages every aspect of recovery and cash posting, streamlining the process to accelerate payments and maximize the recovery of outstanding bills. Utilizing AI and RPA, we analyze payment patterns, prioritize follow-up’s and predict payment delays and denials. These tools also allow us to generate AI summaries for quick, actionable call notes and conduct smart invoice matching with embedded rules and automatic appeal packet annotation for faster resolutions. This comprehensive approach ensures faster cash flow and reduces the time and effort needed to recover unpaid invoices.
- Cash Posting: ERN reconciliation, manual deposits, zero remits, insurance correspondence.
- Denial Management: Identification of denied claims, research, claim resubmissions and appeals. Feedback loop to establish corrective action for preventable denials.
- AR Management: Follow-up on claims with no response and denial follow-ups.
- Special Processes: Month end prep, month end close reports, other custom reports or special processes.
Empowering Home-Based Care: Flexible Partnership Solutions for Revenue Cycle Optimization
Feature List | End-to-End Revenue Cycle Management | Focused Solutions | Expert Staffing |
Prochant provides comprehensive support across the entire revenue cycle | |||
Prochant provides hybrid support through offshore resources and onshore leads | |||
Prochant uses Pulse Connect to streamline workflows and intelligently allocate resources | |||
Prochant provides clients with access to Pulse Analytics to view their analytics dashboard, offering real-time visibility into KPIs | |||
Prochant collaborates with client to determine KPIs, outcomes and workload | |||
Prochant determines staffing levels | |||
Prochant manges one or two aspects of the revenue cycle (intake, billing, or collections) | |||
Prochant manages quality and productivity of resources | |||
Client determines staffing levels | |||
Client is responsible for KPIs, outcomes and work allocation |
Latest News and Insights: Stay Informed, Stay Ahead
For HME providers, revenue cycle management is more than a billing function. It plays a central role in financial stability, operational efficiency and long-term growth. Yet many providers are losing revenue every day due to inefficiencies that often go unnoticed.
In episode 11 of Beyond the Drip, we sit down with Rowena Birnel, President and CEO of Infusion Solutions, to hear one of the most inspiring stories in home infusion.
Prochant PulseIQ™ boosts Prochant’s end-to-end RCM services with intelligent automation, predictive analytics and guided workflows that are all designed to help Prochant’s teams work smarter, faster and with greater accuracy.
